After a long stay in hospital with complex medical needs, that had included a tracheostomy and critical illness weakness, with a severe acute stenosis of the cervical spine also noted; Client A was referred to QEF for intensive multi-disciplinary rehabilitation to optimise independence and functional ability:
Physiotherapy – lower limb strengthening, standing and walking,
Occupational therapy – using upper limb in functional activity
Speech and Language therapy – swallowing rehabilitation and
Psychology – Cognition and Mood
Client–centred Goals:
On arrival at QEF, Client A presented with global weakness, required assistance of two to transfer and complete daily functional activities, assistance of two for all personal care, bed mobility and transfers and relied on a PEG for all nutrition and hydration needs. Their aim was to return home to live with their spouse. Several client-centred and SMART goals were developed for each discipline which included:
– OT: To be independently completing single handed personal care tasks at sink with +/- adaptive aids in 3/52 (achieved.)
– Physio: To be able to mobilise household distances on a single level with the assistance of an appropriate aid.
– Psychology: To monitor mood and use different coping strategies to support with any low mood and anxiety during their stay at QEF.
– SLT: To attend a VF appointment to check swallowing status on X-ray and to progress to a level 7a easy chew diet with strict advice on slowing down and eating safely
– MDT: To partake in meaningful recreational activities both at home and in the community with the appropriate support, such as going out with children and grandchildren.
Treatment Summary
– OT: Client was working on functional and dexterity tasks, upper limb strengthening and stability exercises, plus functional kitchen tasks and techniques for washing and dressing. They also used the Tyromotion for upper limb strength.
– Physio: The client was highly motivated in all physiotherapy sessions and their mobility progressed significantly. They were independently mobile with a standard 4-wheeled walker for approximately 150-200m indoors and able to grasp a standard walker handle due to improved upper limb and grip strength.
– SLT: The client presented with significant pharyngeal sensorimotor dysphagia, related to cervical myelopathy. A PEG tube was in use for all nutrition, hydration and medication. Therapy interventions focused on laryngeal strengthening and slow swallow rehabilitation, to ensure safety at each stage.
– Psychology: The client displayed some anxiety around uncertainty in the future, but was encouraged by the close support of family and the desire to return home. Work was also done to look at changing mindsets and cognitive beliefs towards progress.
– Nursing and care: focus was on working with incontinence until the client was able to access the toilet safely, fitting a nebuliser at night to support respiration and managing medicines through the PEG and then taking medicines safely orally.
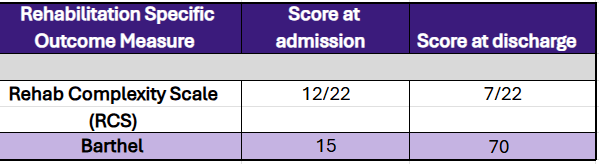
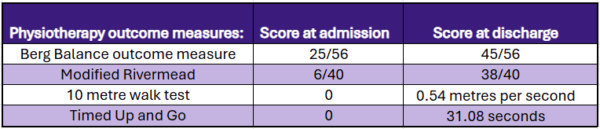
Outcomes
OT: The client progressed to showering using a drop-down shower chair with supervision and a perching stool for personal care at the sink. They required assistance of one for dressing upper body but could dress lower body using adaptive aids with supervision. Thermoplastic custom-made resting hand splints were made for wear during the day.
Physio: Strength generally improved in all aspects of function. Outside, the client was able to mobilise safely with a four wheeled walker. They succeeded in ascending and descending the stairs with bilateral rails and supervision of one. Balance improved considerably and sitting tolerance improved with increased time spent sitting safely and effectively.
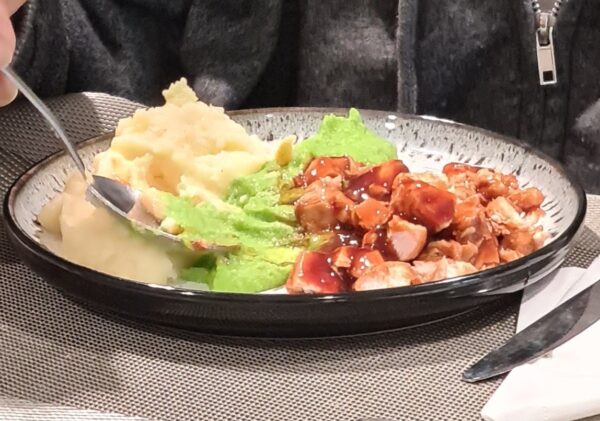
SLT: The client made significant improvements with swallowing. Over 3 months they progressed through all the diet levels (IDDSI) and reached the goal of eating a normal diet and drinking normal fluids, without the cough/clear strategy required to give extra airway protection. PEG tube was no longer needed and all tablets were administered orally.
Psychology: by leveraging the strong family support progress was made in slowly reintroducing the client to daily enjoyed activities.
Conclusion
Overall, the client made significant progress in all outcomes, which was shown in function from initially being significantly affected physically and with the swallowing status, to returning home independently, taking a full normal diet and mobilising with aid.